 Menorrhagia is defined as menstruation at regular cycle intervals but with excessive flow and duration and is one of the most common gynecologic complaints in contemporary gynecology. Clinically, menorrhagia is defined as total blood loss exceeding 80 mL per cycle or menses lasting longer than 7 days. The World Health Organization reports that 18 million women aged 30-55 years perceive their menstrual bleeding to be excessive. Menorrhagia must be distinguished clinically from other common gynecologic diagnoses. These include metrorrhagia (flow at irregular intervals), menometrorrhagia (frequent, excessive flow), dysfuntional uterine bleeding and polymenorrhea (bleeding at intervals <21days).
Menorrhagia is defined as menstruation at regular cycle intervals but with excessive flow and duration and is one of the most common gynecologic complaints in contemporary gynecology. Clinically, menorrhagia is defined as total blood loss exceeding 80 mL per cycle or menses lasting longer than 7 days. The World Health Organization reports that 18 million women aged 30-55 years perceive their menstrual bleeding to be excessive. Menorrhagia must be distinguished clinically from other common gynecologic diagnoses. These include metrorrhagia (flow at irregular intervals), menometrorrhagia (frequent, excessive flow), dysfuntional uterine bleeding and polymenorrhea (bleeding at intervals <21days).Signs and symptoms
§ Useful historical features include: bleeding substantially heavier than the patient’s usual flow, bleeding lasting more than 7 days, flow associated with passage of significant clots Anemia
§ The following symptoms tend to suggest that cycles are ovulatory: regular menstrual interval, mid-cycle pain (mittelschmerz), Dysmenorrhea, premenstrual symptoms - breast soreness, mood changes, etc.
§ Abdominal pain or cramps at other times of the cycle may be associated with structural causes: Myomas, Polyps, Ovarian tumors
§ Hirsutism or acne: may accompany polycystic ovarian syndrome
Mortality/Morbidity
Patients who lose more than 80 mL of blood, especially repetitively, are at risk for serious medical sequelae.
· Menorrhagia is the most common cause of anemia. Women are likely to develop iron-deficiency anemia as a result of their blood loss. This usually can be remedied by simple ingestion of ferrous sulfate to replace iron stores.
- If the bleeding is severe enough to cause volume depletion, patients may experience shortness of breath, fatigue, palpitations, and other related symptoms. This level of anemia necessitates hospitalization for intravenous fluids and possible transfusion and/or intravenous estrogen therapy, or surgical intervention if required to control the menorrhagia.
· Other sequelae associated with menorrhagia usually are related to the etiology. For example, with hypothyroidism, patients may experience symptoms associated with a low-functioning thyroid (eg, cold intolerance, hair loss, dry skin, weight gain) in addition to the effects of significant blood loss.
Causes:
Menorrhagia can be caused by a variety of causes include: Imbalance of hormones (estrogen and progesterone), Fibroids (benign uterine tumors), Pelvic infection, Endometrial disorder, Intrauterine device, Hypothyroidism, Pregnancy, Ovarian cyst or tumor and other hormonal causes.
§ Hypothyroidism
§ Endometrial proliferation/excess/hyperplasia: Anovulation, oligo-ovulation, Polycystic ovarian disease (PCOD), Ovarian tumor, Obesity, Hormone (estrogen) therapy
§ Endometrial atrophy: Postmenopause, Prolonged progestin or oral contraceptive administration
§ Local factors: Endometrial polyps, Endometrial neoplasia, Adenomyosis/endometriosis, Uterine myomata (fibroids), Intrauterine device (IUD), Uterine sarcoma
§ Coagulation disorders: Thrombocytopenia, platelet disorders, von Willebrand disease, Leukemia, Ingestion of aspirin or anticoagulants, Renal failure/dialysis
Medications:
Drugs of choice:
§ For acute control of severe bleeding: Estrogen, conjugated (Premarin)
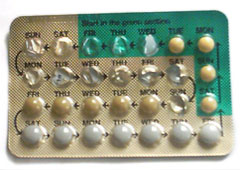
§ For less severe bleeding or after control of acute bleeding: Medroxyprogesterone acetate (Provera), any combination oral contraceptive, (usually one of the “high dose” oral contraceptives)
§ To prevent heavy bleeding in subsequent cycles: Medroxyprogesterone acetate, usual cyclic dose of a combination oral contraceptive
§ For endometrial atrophy in postmenopausal woman: Estrogen plus progesterone replacement therapy
*Please refer and consult with the physicians or pharmacists for contraindications and precautions of the medicines suggested.
Alternative Drugs
§ Non-steroidal prostaglandin-synthetase inhibitors (naproxen, mefenamic acid, ibuprofen, and others) can reduce blood loss with ovulatory cycles and reduce dysmenorrheal, Norethindrone acetate (Aygestin) during the assumed latter half of menstrual cycle, Danazol and GnRH, Megestrol acetate (Megace) to prevent progression to endometrial carcinoma and to treat atypical hyperplasia


 Women on a diet or women who are conscious of their weight and figure always display a certain fear of chocolate. They avoid it like plague, thinking that the sugar and the calories that chocolate contains will make their diet and weight-loss plans go haywire. And yet, when things go wrong and they are feeling down, they go and raid the fridge and gobble on as much chocolate as they can. When these women come to their senses later on, they feel horribly guilty and try to burn the sugar and calories gained from the binge.
Women on a diet or women who are conscious of their weight and figure always display a certain fear of chocolate. They avoid it like plague, thinking that the sugar and the calories that chocolate contains will make their diet and weight-loss plans go haywire. And yet, when things go wrong and they are feeling down, they go and raid the fridge and gobble on as much chocolate as they can. When these women come to their senses later on, they feel horribly guilty and try to burn the sugar and calories gained from the binge. 


